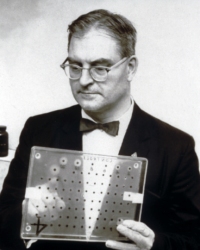
January's Spotlight is on Robert Guthrie, MD, PhD. Dr. Guthrie introduced the first newborn screening test in the United States for phenylketonuria (PKU) in the early '60s and the use of the Guthrie card to collect the heel stick blood for newborn screening is now standard. Dr. Guthrie began his clinical career as a cancer research doctor but became interested in preventing mental retardation after his second son John was born with developmental disabilities and his niece was diagnosed with PKU.
In 1957, Guthrie met Dr. Robert Warner, director of the Children's Rehabilitation Center of Buffalo. Dr. Warner was treating children with PKU by restricting dietary phenalalanine but was having trouble measuring blood phenylalanine levels because he had to send the samples all the way to a firm in California each time he tested a patient. Dr. Warner proposed that Guthrie devise a simpler method of measuring blood phenylalanine. After only 3 days, Guthrie developed a a simple method of monitoring blood phenylalanine that involved only a few drops of blood. The principle was identical to that of the bacterial assays he had used for cancer patients. He called the technique "bacterial inhibition assay". For testing phenylalanine, he used a spot of blood on a filter paper disc that he put on the surface of an agar culture gel, which contained a specific substance to inhibit the growth of bacteria, but which was reversed by phenylalanine. If excess phenylalanine was present in the blood, it removed the growth inhibition and bacteria grew. After overnight incubation he could examine the sample and compare the diameter of the growth zone around it with that of a "control" disc of blood to which he had added known quantities of phenylalanine. The agar remained clear except for circles of growth surrounding the discs that contained phenylalanine.
It soon became clear that in the case of PKU, the sooner the diagnosis was made and treatment begun, the better the prognosis for normal intellectual growth. It was at this point that Guthrie sought ways to simplify his test. His first attempt proved to be more successful than he could have hoped. He found that he could blot a piece of filter paper directly on a small heel puncture wound, dry the blood sample and then punch out a small disc from the blood spot and proceed as usual with the rest of the test. He could hardly believe his good luck.
In order to put his technique to a test, Dr. Guthrie got permission to test some 3,000 residents of a state school for the retarded near Rochester. The administrators at the school maintained that all of their residents had been tested with the ferric chloride urine test, however Bob found 23 cases of PKU, four more than had been diagnosed by urine testing. By the fall of 1961 Guthrie was convinced that all infants should be tested before they left the hospital and his determination was almost unstoppable.
In 1961, Dr. Guthrie and his laboratory began receiving filter paper specimens of blood from newborn infants in two Jamestown hospitals. With the demand evident, Dr. Guthrie received funding from the United States Children’s Bureau to try screening on a national basis for PKU in newborns. This gave Dr. Guthrie the resources to establish a factory within a small house next to the Buffalo Children’s Hospital to prepare material for the PKU screening test. Within two years, 400,000 infants had been tested from 29 states, resulting in no less than 39 positive cases of PKU. Newborn screening for PKU identified an incidence of almost one in 10,000 births in the United States. Importantly, no cases were missed by this new method of screening, allowing for definitive therapy to be given to all identified patients before neurotoxicity set in.
Impressed by Dr. Guthrie’s successes, and driven by Dr. Guthrie’s own determination, the National Association for Retarded Children lobbied for a legally mandated PKU screening throughout the mid 1960s. In 1967, 37 states passed laws mandating PKU screening in all newborns; today, all 50 states have such laws. The greatest success of the development of PKU newborn screening is that it precipitated people to ask whether other diseases may be prevented through similar and parallel early detection methods. It soon became clear that they could, and by the late 1960s, newborn screening for genetic diseases became a part of infant health care in the United States. Most newborn screening programs in the United States now use tandem mass spectrometry (MS/MS) as the principal tool to analyze blood spots. Before tandem mass spectrometry, separate assays (eg, bacterial inhibition assays) were needed for each possible metabolic disorder, in addition to tests for endocrine and hemoglobin disorders, to name a few. The menu of diseases identified by newborn screening continues to expand today, with cystic fibrosis most recently added to the diseases screened for by most states.
Dr. Robert Guthrie died on June 23, 1995, at the age of 78. He was married to his wife for 53 years, with whom he had six children. Expanded newborn screening programs based on Dr. Guthrie’s blood collection system for early detection of treatable diseases continues today as the stepping stone for improved children’s health in the United States and the world.
Sources
Gonzalez, J, and Willis, MS. "Robert Guthrie, MD, PhD; Clinical Chemistry/Microbiology." Lab Medicine. 2009; 40(12): 748-749.
Holt Koch, Jean. "History of PKU - Origins." The World of PKU. Web. 21 Dec. 2012.